COVID-19, How Do I Save My Practice?
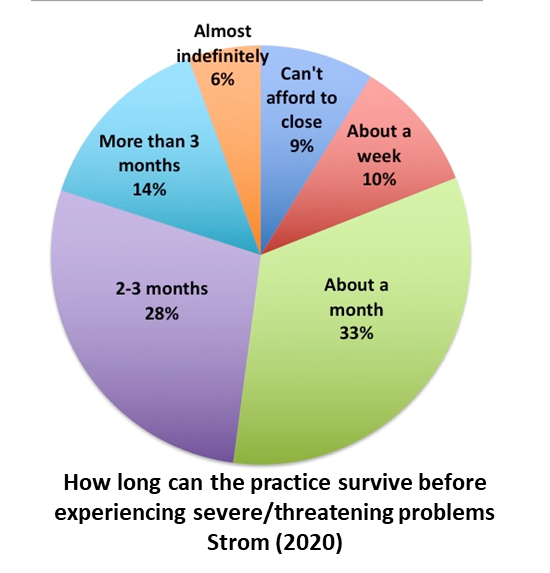
While COVID-19 is a serious disruption of clinical income, there have been many storms before and there will be many more after this one. This is not total disaster, especially for an established practice. During the week of March 18-24, 2020, Strom (2020) conducted a poll to review the actual situation for clinic owners. The small sample of 220 notwithstanding consisted of 69% private practice hearing care professionals. By the end of the survey, 71% of the clinics surveyed were either working fewer hours or not seeing patients and 95% of the reduction in patient care was due to COVID-19. In Strom’s poll of clinics, most anticipate a sales decrease of almost 90% and are scaling back their operations to accommodate the drastic reduction in gross revenue.
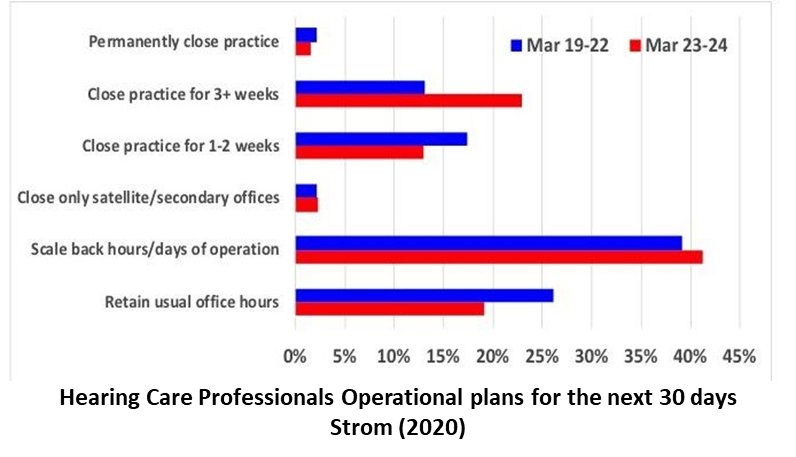
While less than 5% will permanently close their doors due to the virus, those that remain operational will modify procedures and protocol to continue to work with their patients. Specifically, the practitioner needs to determine what adjustments to the practice need to be instituted now that the government has issued orders such as “Shelter in Place,” “Stay at Home,” “Social Distancing,” and only travel for “essential services”, such as groceries, medical treatment, pharmacies, gas, etc. While it is debatable as to whether hearing care is essential, the err should be on the side of our patients as well as the clinicians that see them.
What Are Practitioners Doing to Save their Practices?
Many practitioners are asking: “what do I do?” Kasewurm (2020), in successful practice for over 30 years, answers with, “You do what we as business owners always do when faced with obstacles – we buckle in and get ready to ride it out. We use the time wisely to prepare for what is sure to be a recovery.”
Patient Care
Of course those practices that remain open should follow the CDC Guidelines for Disinfecting for Healthcare Clinics (2008) and the U.S. Coronavirus Guidance (March 23, 2020) which has been extended to April 30, 2020. The patient care suggestions in the following figure are certainly not an exhaustive list of considerations for treatment in this time of disaster, but include some worthy ideas, even if they merely reinforce some of the procedures that the practice is already conducting.
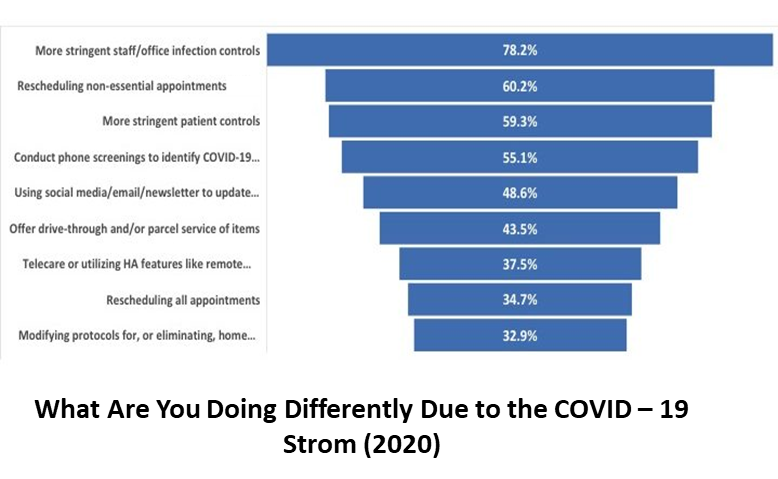
 Some, roughly 35% or so, may feel that there is nothing to do but lock the doors until COVID-19 is no longer a threat. These practitioners may be leaving behind a tremendous opportunity to serve their patients and build trust that can last for years to come. Patients will need care, some more than others, and the ultimate in practice differentiation is how practitioners handle this COVID-19 situation. Since there will likely be minimal to no new business, for the 65% or so of those that remain, patient support will become an area of concentration. The question then becomes how the practice safely provides that support. Front line clinicians know the everyday difficulties experienced by patients will still occur. The hardest hit will be those without close relatives, the very elderly, and those with co-morbid conditions.
Some, roughly 35% or so, may feel that there is nothing to do but lock the doors until COVID-19 is no longer a threat. These practitioners may be leaving behind a tremendous opportunity to serve their patients and build trust that can last for years to come. Patients will need care, some more than others, and the ultimate in practice differentiation is how practitioners handle this COVID-19 situation. Since there will likely be minimal to no new business, for the 65% or so of those that remain, patient support will become an area of concentration. The question then becomes how the practice safely provides that support. Front line clinicians know the everyday difficulties experienced by patients will still occur. The hardest hit will be those without close relatives, the very elderly, and those with co-morbid conditions.
 Some clinics in non-locked down areas are offering “drive through” device support (AAA Board of Directors (2020)). If there are patients that require services, someone in the office could meet a patient at their car, the staff member can have a tray (covered with a sheet that can be disposed of) where the person deposits their hearing aid (or other device) from within the car. The hearing aid can be cleaned/restored to function and then delivered back to the car. This procedure can minimize patients encountering each other or staff members while in the waiting room. Although these mostly non-revenue services are certainly not part of our traditional clinical roles, this extra caring and service builds trust that will long be remembered, not just by the patients, but by many others as well.
Some clinics in non-locked down areas are offering “drive through” device support (AAA Board of Directors (2020)). If there are patients that require services, someone in the office could meet a patient at their car, the staff member can have a tray (covered with a sheet that can be disposed of) where the person deposits their hearing aid (or other device) from within the car. The hearing aid can be cleaned/restored to function and then delivered back to the car. This procedure can minimize patients encountering each other or staff members while in the waiting room. Although these mostly non-revenue services are certainly not part of our traditional clinical roles, this extra caring and service builds trust that will long be remembered, not just by the patients, but by many others as well.
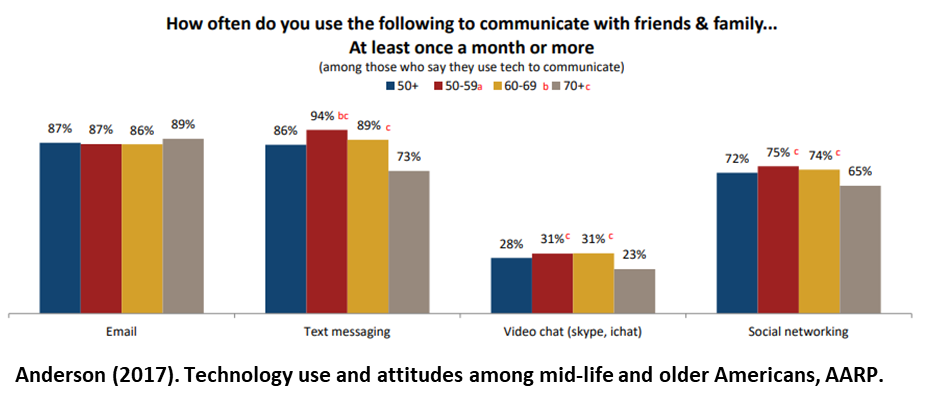
For the younger group of Baby Boomer patients, it is a bit easier to provide follow-up care with computers and smart phones, as more than 90% of those age 50 and over routinely use computers and high-level internet technology. An AARP study by Anderson (2017) indicates that a substantial number of these individuals use computers and conduct much of their business on smart phones through apps, email, and texting. There is likely even more than presented in this study, as thousands have turned 65 in the past 3 years since this study was completed. Thus, communication with email and texting is normal, and even FaceTime can be useful with this group.
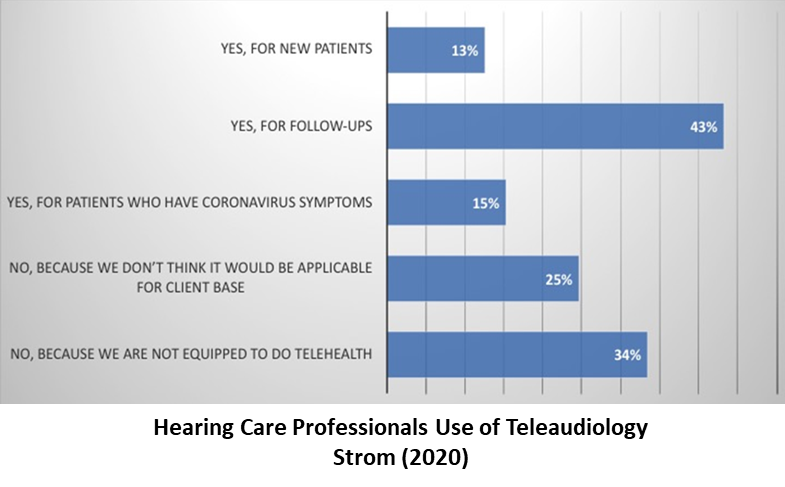 While discussed for decades, Teleaudiology for overall hearing care is still in its early stages and, for the most part, primarily limited to counseling. Although there are some screening tests that can be conducted using Teleaudiology, for the most part, the various systems and websites that can be used for these services are primarily for physicians. The sites that are used by physicians allow them to conduct interactive treatment by diagnosing disorders and prescribing medication in an environment that allows for billing. For Teleaudiology during the COVID–19 outbreak, online hearing screening will not be the primary concern, and most manufacturers do not have remote capabilities for programming devices. Those that do only offer limited adjustments. Thus, if it is a follow-up visit limited mostly to counseling, according to the survey, it could be used 71% of the time but will likely produce minimal revenue. At the very least, call all your patients, even if it is 20-30 patients per day. You will be differentiating your practice by relationship.
While discussed for decades, Teleaudiology for overall hearing care is still in its early stages and, for the most part, primarily limited to counseling. Although there are some screening tests that can be conducted using Teleaudiology, for the most part, the various systems and websites that can be used for these services are primarily for physicians. The sites that are used by physicians allow them to conduct interactive treatment by diagnosing disorders and prescribing medication in an environment that allows for billing. For Teleaudiology during the COVID–19 outbreak, online hearing screening will not be the primary concern, and most manufacturers do not have remote capabilities for programming devices. Those that do only offer limited adjustments. Thus, if it is a follow-up visit limited mostly to counseling, according to the survey, it could be used 71% of the time but will likely produce minimal revenue. At the very least, call all your patients, even if it is 20-30 patients per day. You will be differentiating your practice by relationship.
Training and Other Clinic Modifications
In an independent practice, there are always things to do when the practice is slow. With all the other duties of practitioners, it makes sense that about 60% of the clinics have chosen to reduce their hours rather than totally close as of this week (March 27, 2020). While there is still uncertainty as to how long and how deep the COVID-19 virus will affect clinical operations, it is a great time to consider possible modifications to the practice. If funds are available, now might be the time to have the staff go through that Audiology Assistant Training, or for clinicians to become more involved in tinnitus and/or balance assessment and treatment. Several sources offer highly recognized, relatively inexpensive online courses to obtain new valuable skills or CEUs that may be helpful in the future. The new skills offered might lead to operational changes that provide new profitable services to the community when the practice limitations are lifted.
Now might be the time for new equipment, to increase the array of products, or to add scanning technology that could modernize diagnostic procedures, further differentiating the practice for when the sanctions are lifted. If contractors are still available in the area, it might be the time to consider a clinic facelift, to include new carpet or furniture, updated decorations, and other physical modifications that create the best impression of the practice. Administratively, there is always the next print, social media, direct mail, or open house marketing campaign that be prepared.
The Business Side – How Do I Know What to DO?
Many long-time practitioners recognize that it is only a matter of time when COVID-19 will pass, and clinics will be back in business. For now, though, the concerns of practitioners are as follows:
- How do I pay my employees?
- Do I lay them off? If so, which ones?
- How do I pay the rent?
- How do I pay my business loan?
- How do I pay the accounts payable?
- Will my receivables be able to pay?
- How do I keep the patients that are in my database after the virus dilemma?
- Do I have enough defensive assets, or do I need a loan?
- How do I plan for the future?

The First Line of Defense
While COVID-19 is not a hurricane, tornado, or flood event, it is a total business disaster that requires the use of the practice’s first shelter - the defensive assets (business savings account). These are funds that are typically put away during good business times for those that are interrupted by natural disasters. The results of the Strom survey indicated that about 48% of the those polled had enough defensive assets to stay in business without any revenue for at least 2 -3 months. These are practices that have prepared for disaster, not knowing when or if it will come.
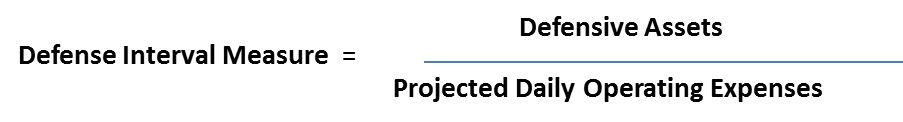
Technically, the calculation is the Defense Interval Measure (DIM) (Traynor, 2018). Thisis an easy calculation that determines how long these defensive assets will sustain the practice without any external cash flow:
The formula for the DIM is as follows:
To compute the DIM, there are some things that must be known. First, the practice must know the amount of funds that can be used for defensive purposes. To calculate the length of time that the practice can open its doors in an emergency, it is necessary to consider the Projected Daily Operating Expenses (PDOE). The PDOE is calculated by the following formula:
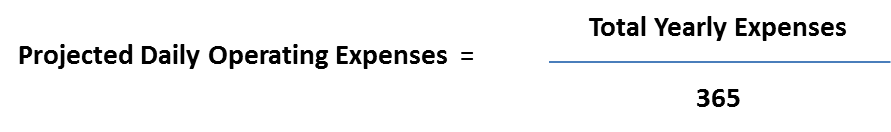
To arrive at the PDOE, simply go to the selling, general, and administrative expenses located on the income statement and find the total yearly operating expenses. For this example, let’s say that our total yearly expenses are $311,000. The total yearly expenses of $311,000 are then divided by 365 as presented below:
In this example, it costs the practitioner $852 to stay open each day. If the practitioner has $50,000 available in Defensive Assets, then the practice’s Defensive Interval Measure would be 58.7 days. To meet the recommended DIM of a minimum of 90 days the practitioner in this example would need $76,680 in total.
While there are other methods of computation, this one is easily conducted and offers an estimate of how long the business assets will sustain the practice.
Detailed Assessment of the Practice and its Future
If there are minimal to no defensive assets, it is necessary to make a detailed review of the effects the business reduction or closure has had and will have on the future of the practice. This detailed analysis can answer many of the above questions, as well as reduce anxiety for the practice owner. As a small business specialist, Parsons (2020) suggests that there are five things that should be done:
- Build a business forecast with multiple scenarios
- Examine expenses
- Assess staffing plan, adjust if necessary
- Forecast cash flow
- Apply for a loan
Build a Forecast with Multiple Scenarios
 Before sophisticated web sites and computer programs were available, business forecasts were difficult to produce. Now, with the help of Excel or even task-specific programs like LivePlan (https://liveplan.com) combined with solid historical practice information from your practice management and accounting software, you can project financial results for various scenarios to help you prepare. This process allows the practitioner to review the worst, medium, and best-case scenarios by manipulating certain variables such as expenses, employees, revenue and other variables. If there is a shortfall in the bottom line, these forecasts can also assist practitioners in determining of the amount of a loan that would be necessary to continue operations.
Before sophisticated web sites and computer programs were available, business forecasts were difficult to produce. Now, with the help of Excel or even task-specific programs like LivePlan (https://liveplan.com) combined with solid historical practice information from your practice management and accounting software, you can project financial results for various scenarios to help you prepare. This process allows the practitioner to review the worst, medium, and best-case scenarios by manipulating certain variables such as expenses, employees, revenue and other variables. If there is a shortfall in the bottom line, these forecasts can also assist practitioners in determining of the amount of a loan that would be necessary to continue operations.
Examine Expenses
There are many areas where expenses can be trimmed. Determine which expenses are essential and which are not. Now is the time to negotiate with landlords, leasing companies, and other vendors for modifications of their costs to you. They are eager to have you as a customer and are usually willing to negotiate modifications in their usual costs relative to the perceived reduction in clinic income. While you cannot expect these expenses will go to zero, it is reasonable to ask for a reduction.
Employees
Employees are the most expensive cost within the practice. While the tendency would be to keep the total force of employees, the reduction in patient traffic and the revenue that they create may require modifications. It may be that layoffs are necessary or a reduction in the hours worked per day are required to keep the practice in business and/or prepare for recovery. Before deciding on altering employee compensation, hours, or employment, owners should be sure to review the various government relief programs coming online to ensure the best long-term decision is being made for the practice.
Summary
A cash flow budget is an estimate of all cash receipts and all cash expenditures that are expected to occur during a certain time period. Estimates can be calculated monthly, bimonthly or quarterly. Cash flow budgeting looks only at money movement, not at net income or profitability. A cash flow budget is a useful management tool because it:
- Forces you to think through your plans for the year.
- Tests your business plan to see if there is enough income to meet all your cash needs.
- Projects how much operating credit you will need and projects when loans can be repaid.
- Provides a guide against which you can compare your actual cash flows.
- Helps you communicate your business plan and credit needs to your lender.
Formulation of Cash Flow
 There are some simple issues to consider in this time of the COVID-19 disaster to audiology practices. Watch out for your patients and, within the COVID-19 guidelines, give them the same care that you always have. Analyze expenses and employee situations and, most of all, conduct some forecasts to prepare for possible loans, possible grants or determine if you can survive without borrowing by using your defensive assets.
There are some simple issues to consider in this time of the COVID-19 disaster to audiology practices. Watch out for your patients and, within the COVID-19 guidelines, give them the same care that you always have. Analyze expenses and employee situations and, most of all, conduct some forecasts to prepare for possible loans, possible grants or determine if you can survive without borrowing by using your defensive assets.
In the words of Prince Charles who recently tested positive for COVID-19:
“There is nothing like a jolly good disaster to get people to start doing something.”
Get the COVID – 19 Private Practice Playbook from Pivot Hearing
Oftentimes, a partner to walk you through this process - who has the experience of working with hundreds of practices nationwide and familiarity with all the tools of the industry - is helpful to get you started or to prepare information for you to make informed decisions. Pivot Hearing is ready to help you through this process and has already developed a COVID-19 Private Practice Playbook to help guide you during this time. They stand ready to support and are committed to doing everything they can to help sustain independent hearing practices.
About the Author
Robert M. Traynor, Ed.D., MBA, FNAP, is a Practice Consultant for Pivot Hearing. For 45 years, Dr. Traynor practiced audiology at Audiology Associates, Inc., Greeley, Colorado, providing diagnostic & rehabilitative treatment for hearing loss and tinnitus as well as interoperative monitoring.
References
- AAA Board of Directors (2020). COVID-19 and Our Audiology Practices, American Academy of Audiology, Reston, VA.
- Anderson, G. (2017). Technology use and attitudes among mid-life and older Americans. American Association of Retired People (AARP), Retrieve March 26, 2020.
- Ehrenfeld, T. (2019). Need an audiologist but can't travel? Telehealth may be an option. Healthy Hearing, July, Retrieved March 26, 2020.
- Hearing Review (2020). Critical Steps in Establishing a Teleaudiology Practice, Hearing Review, Retrieved March 25, 2020.
- Kasewurm, G. (2020). HELP! I Don’t Know What to Do Next!. Dr Gyl’s Blog. Retrieved March 26, 2020.
- Strom, K. (2020). Hearing Review Coronavirus impact survey results (March 19-24). Hearing Review, Retrieved March 27, 2020.
- Traynor, RM (2018). Chapter 11: Fiscal Management & Accounting. In R. Glaser & R. Traynor, Strategic Practice Management, San Diego: Plural Publishing.
- Traynor, RM (2019). Chapter 4: Accounting for Audiologists. In B. Taylor, Ed, Audiology Practice Management. New York: Thieme Medical Publishers